ANTIMICROBIAL RESISTANCE
Antimicrobial resistance means resistance to drugs for infections that are caused by bacteria, viruses, parasites, or fungi. A growing list of infections – including pneumonia, tuberculosis, blood poisoning, gonorrhoea, many skin and wound infections and foodborne diseases – are becoming harder, and sometimes impossible, to treat. New resistance mechanisms are spreading in all parts of the world, leading WHO to call antimicrobial resistance an “invisible pandemic”.
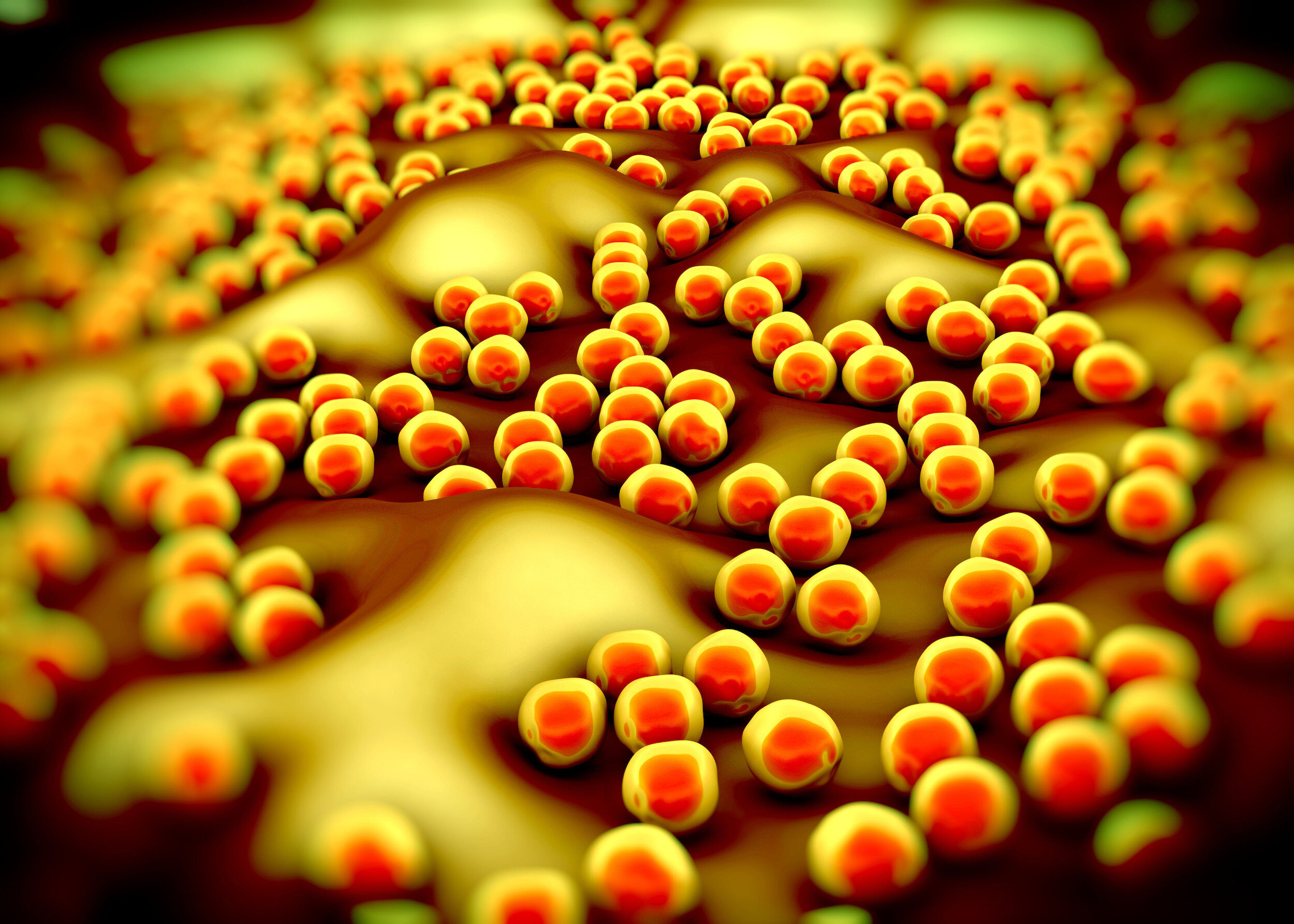
We have entered the age of the superbugs.
“We are already starting to see signs of a post-antibiotic era, with the emergence of infections that are untreatable by all classes of antibiotics. Antimicrobial resistance is an invisible pandemic.”
Antibiotic resistance is currently responsible for 700,000 deaths a year. The World Health Organisation estimates that this could grow to ten million deaths a year by 2050 if no action is taken: that’s more deaths than cancer.
In the words of Professor Dame Sally Davies, when she was Chief Medical Officer: “The world is facing an antibiotic apocalypse.” Unless action is taken to halt the practices that have allowed antimicrobial resistance to spread, and ways are found to develop new types of antibiotics, we could return to the days when routine operations, simple wounds or straightforward infections could pose real threats to life, she warned.
Overuse, underuse and misuse of antibiotics by humans in healthcare, farming and agriculture have contributed to the crisis, as well as irresponsible disposal of industrial waste, leaching antibiotics into streams and rivers.
Two in three Europeans are still unaware that antibiotics are ineffective against viruses. And consumption of antibiotics by patients who either don’t need them, or who don’t finish their prescribed course, is only part of the problem.
Almost 75% of the world’s antibiotics are now used on animals. In the US, it’s 80%. These drugs are used to boost growth rates and prevent infection. As a result, antibiotic resistance in farm animals is rocketing.
In developing countries, resistance has trebled since 2000. India and China have the highest levels of antimicrobial resistance, which is a major concern as the Asian continent is home to more than half the world’s chickens and pigs.
Added to this, the exchange of resistance genes from animals to humans is much greater than previously thought. We can contract antibiotic resistance from the food we eat.
The last new class of antibiotic was developed in 1987. Many of the big pharmaceutical companies have pulled out of antibiotic research altogether.
This lack of investment is because the market-based approach doesn’t work: antibiotics have a short lifespan and increasingly restricted use, combined with a very high cost. It takes between ten and twenty years to develop a new drug, and the failure rate in research trials is high. We need a different model.
Yet we keep on consuming them. And the more we consume, the faster the bacteria adapt, and develop resistance.
“Antibiotic resistance has long been a problem, but the threats we face are real, immediate, and demand immediate action. Antibiotic resistance threatens modern medicine: our ability to safely perform routine surgeries and complicated organ transplants, as well as chemotherapy, all rely on the ability to prevent and treat infections.”
Dr. Jesse Jacob, Emory University School of Medicine, Atlanta
“Antimicrobial resistance is one of the most urgent health risks of our time and threatens to undo a century of medical progress.”
ReAct: the global threat of antibiotic resistance
https://www.reactgroup.org/antibiotic-resistance/the-threat/
UN reports on drug-resistant infections
https://www.who.int/en/news-room/fact-sheets/detail/antimicrobial-resistance
https://www.who.int/antimicrobial-resistance/interagency-coordination-group/final-report/en/
Difficulties of developing new antibiotics
https://www.bbc.co.uk/news/health-41693229
UK government report on antibiotic resistance action plans
https://www.gov.uk/health-and-social-care/antimicrobial-resistance
Article on alternative public funding model for antibiotic research & development
https://theconversation.com/big-pharma-has-failed-the-antibiotic-pipeline-needs-to-be-taken-under-public-ownership-126058?utm_source=twitter&utm_medium=twitterbutton
Further reading
Superbugs, the Race to Stop an Epidemic by Matt McCarthy
Drug-resistant bacteria ― known as superbugs ― are one of the biggest medical threats of our time. Here, a doctor, researcher, and ethics professor tells the exhilarating story of his race to beat them and save countless lives.
Rising Plague by Brad Spellberg, MD
An inside view from a chief medical officer & medical director of biosciences about the global threat from deadly bacteria and our dwindling arsenal to fight them.